The Disease
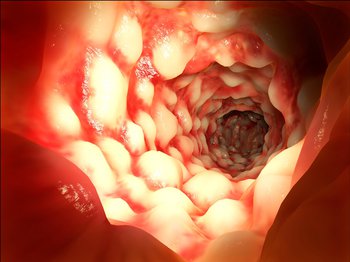
Ulcerative Colitis (“UC”) is a chronic, inflammatory disease that causes sores or ulcers in the lining of the large intestine (the colon).
It is characterized either as “active disease”, where a patient has clinical symptoms of the disease, or “in remission”, periods without clinical symptoms.
Ulcerative Colitis can be further described by the location of the inflammation and sores (ulcers).
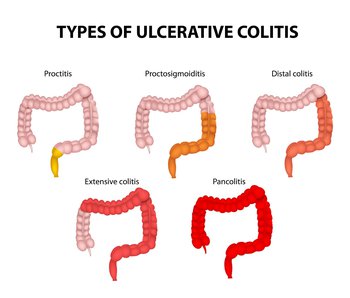
PROCTITIS
Disease is limited to the rectum
PROCTOSIGMOIDITIS
Involves inflammation of the rectum and the sigmoid colon, the next colon region up inside the body
DISTAL or LEFT-SIDED COLITIS
Involves inflammation of the colon up to the splenic fixture (where the colon turns sideways)
EXTENSIVE COLITIS
Inflammation now includes the part of the colon that goes across the body, called the transverse colon. Enemas alone cannot reach all of the diseased parts of the colon with Extensive Colitis.
PANCOLITIS
Refers to inflammation affecting the entire colon
- Ulcerative Colitis affects approximately 750,000 patients in the United States and 6 million patients worldwide.
- The onset of UC is usually diagnosed in patients between the ages of 15 and 30 years, with a second peak in incidence between 50 and 75 years of age.
- Men and women are equally affected by UC.
Symptoms of Ulcerative Colitis
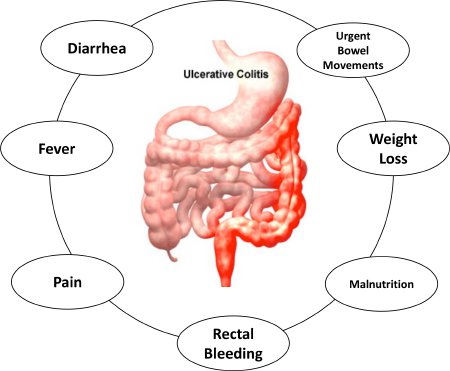
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. Signs and symptoms may include:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- Rectal pain
- Rectal bleeding — passing blood with stool
- Urgency to defecate
- Inability to defecate despite urgency
- Weight loss
- Fatigue
- Fever
Most people with ulcerative colitis have mild to moderate symptoms. The course of ulcerative colitis may vary, with some people having long periods of remission.
More severe symptoms include malnutrition, stunted growth (in pediatric cases), and an increased risk of colon cancer.
Current Treatment of Ulcerative Colitis
There is no known cure for UC. Options to manage the symptoms of UC include 5-ASA (aspirin-like drugs, for mild cases), corticosteroids and immunomodulators including biologics (for moderate to severe cases). These products can be delivered via mouth in the form of a pill, rectally in the form of a suspension enema or suppository, or via injection or IV.
While 5‐ASA is fairly benign, biologics (immunosuppressing drugs) can lead to severe side effects including tuberculosis, skin cancer, or lymphoma. Regardless of the treatment option, 20-30% of UC patients are unresponsive to any drugs and have no alternatives except to undergo colectomy (removal of the colon), a major surgery that leads to challenging, lifelong lifestyle changes.
The treatment of active UC has historically been aimed at reducing symptoms. When the symptoms disappeared, many practitioners believed that the lining of the colon (the mucosa) was healed, without endoscopic confirmation.
Mounting evidence suggests that treating symptoms alone may not be sufficient to achieve optimal long-term outcomes (e.g., fewer complications, procedures, and hospitalizations), and that targeting mucosal inflammation and associated tissue damage (i.e., achieving mucosal healing) may be equally important.
Although complete mucosal healing is a desirable objective of treatment, few studies have included it as a goal of treatment. This results from the reliance on symptoms as a marker of disease activity.
The situation appears to be changing, however, as new data suggest that mucosal healing may be a reliable indicator of treatment efficacy and a key predictor of long-term outcome.